Over the past 16 years, the Boston AF Symposium has earned a reputation for excellence. Dr Jeremy Ruskin, the meeting’s senior director and founder, squeezes more learning into three days than would seem possible. It’s a mystery how he gets that many of Earth’s greatest AF-doctors to Boston in January.
Though this year’s edition coincided with a blizzard, I made it to the waterside conference center just in time.
Here are a few highlights:
AF-Ablation news:
In ablating intermittent (paroxysmal) AF, the big story was that AF-recurrence rates after an initially successful ablation are way too high. All AF-doctors are struggling with this reality, and we all hate that phone call form the post-ablation patient who has recurrent AF.  In most cases, AF comes back after ablation because the burns were not durable. But why not? Unfortunately, for this answer, we will have to wait. People have ideas but no one has definite answers.
Except, of course, Medtronic argues that they may own a better tool for ablating AF.

For the first time ever in adult ablation, freezing may have a fighting chance against burning. Medtronic’s recently released cryo-ablation balloon catheter (Arctic Front) looked quite promising. When the Stop-AF trial was released earlier this year, the primary concern of freezing in the left atrium was safety. What I heard, from experts that I respect, like the outspoken Karl-Heinz Kuck from Hamburg, Germany, was that the feared complications of cryo-ablation–phrenic nerve injury and PV stenosis–can be largely avoided by simple technical maneuvers in the EP lab. I look forward to earning more about this new technology.
In ablating long-standing (permanent) AF, the major story was that there are far more questions than answers. Perhaps the meeting’s most lively debate was on how best to ablate chronic AF?  The choices spanned the entire spectrum of aggressiveness: from the minimalist approach of the University of Pennsylvania group, who isolate the PV areas, any ancillary triggers and that’s it; through the stepwise Bordeaux approach which calls for PV isolation plus lines in the left atrium until AF organizes into something focal that can then be ablated; to the most aggressive, burn-every-left-atrial-signal approach advocated by the group in Austin Texas.
In the end of the ablation sessions, there were many questions and few answers:
- Are the minimalists burning enough?
- Are the aggressors burning too much? (If the entire left atrium is ablated and cannot contract, then what good is sinus rhythm?)
- How can Dr Pappone be so successful? Â Is there magic to be had in Milan?
- Is there a role for collaboration with cardiac surgeons?
- And of course, as it is every year, a voice from the distant microphone in the back of the hall asks Dr Natale whether he would undergo the extensive ablation that he advocates? His answer is always the same: “…let me know how you feel about ablation when you get AF.”
Stroke prevention:
Stroke prevention in AF means dealing with blood clots that form in the left atrial appendage. The LA appendage has nooks and crannies that, in the presence of a non-contractile fibrillating atrium, act as excellent sources of clot formation. When these clots dislodge they often travel north to the brain and cause devastating strokes. There are two ways to approach LA clots: with blood thinners, or exclusion of left atrial appendage.
Until this fall, the only medical option to prevent strokes in AF was warfarin. Now, in non-valvular AF, we have the novel new warfarin-substitute, dabigatran (Pradaxa). It was surprising to hear that more than one expert suggested that all patients with non-valvular AF should be offered the new drug–even those doing well on warfarin. That’s a tough call at the moment, but without doubt dabigatran looks like a potential blockbuster.
We also heard that Boehringer’s monopoly will not last long. There are other blood thinners on the horizon. Look for the Factor Xa inhibitors, rivaroxaban, apixoban and edoxaban, to be approved in the near-term. In total, these new blood-thinners will eventually replace warfarin. Thank goodness.
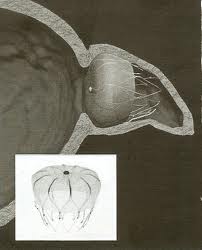
Another cool feature of the Boston AF symposium is that it always looks far into the future. For stroke prevention, the future may include devices that occlude, tie-off and otherwise remove the left arial appendage. Co-course director and incessant tinkerer with cardiac devices, Dr Vivek Reddy showed some dazzling examples of LA appendage isolation devices. He always shows such devices, but this year, it looked like some of these gadgets are approaching prime-time, or said another way, something I could do.
Miscellaneous Notes:
- There were no words uttered on dronedarone. Not even from those who touted it so highly the past few years, and not even after the two cases of liver failure were reported on Friday. The ancient drug, Mexiletine, was mentioned during a case presentation, but not dronedarone. Silence.
- Dr Maurits Allessie–of AF begets AF fame–has presence. It was cool to be in the same room with a legend. For that matter, though I can’t always understand them, the basic scientists are a refreshing bunch who add a great deal of credibility to this meeting.
- Eric Prystowsky continues his run as the most entertaining speaker. His irreverence towards epidemiologists, statisticians and non-clinician scientists, especially those responsible for the recently published and now infamous JAMA ICD article, was very well received. He makes you grin and teaches at the same time.
I am already looking forward to next year’s conference.
The year in AF will be exciting. Â Look for reports on our actual experience with the cryo-balloon, approval of another blood thinner to compete with dabigatran, and perhaps some more information on increasing the durability of RF lesions.
JMM
13 replies on “Highlights of the 2011 Boston AF Symposium”
How is something like the cryo-balloon tested? Rats? Cadavers? How does a doctor recruit people with AF to be the first to use the technology? How does one convince people to do that?
Allison,
Your first question is easy…Most medical devices begin their testing in an animal lab. In the case of the cryo-balloon, Dr Kuck pointed out that his group published a series of 346 patients in 2008, in the Journal of the American College of Cardiology. So even before the Stop-AF trial was publicized this year, there was already ample European data on cryo. In that paper, they pointed out that almost all the cases of phrenic nerve damage occurred with the smaller (23mm) balloon–which Dr Kuck says should never be used.
Your second question is really hard. It implies the notion of the ‘learning curve’; a topic that Dr Gawande talks about in his book Complications. The concept is that doctors get better with repetition and experience, but gathering this experience means there has to be patients 1-50 (or so.)
I think the way proceduralists and surgeons justify using new tools on real patients are that these tools represent incremental changes to the procedure, not an entirely different procedure altogether. For instance in the case of the cryo-balloon, the guts of the ablation procedure are the same: placement of catheters, trans-septal, identification and electrical isolation of the pulmonary veins, etc. Moreover, AF-ablation can be ablated faster and with fewer complications in 2011 primarily because of familiar tools that–one day in the past–felt unfamiliar.
Thanks.
A wonderful synopsis of the meeting. Thanks. Try to attend this meeting each year, but couldn’t do so this time. No problem: can always rely on ‘DrJohnM’s blog’ for providing the next best thing!
Kind words feel nice. Thanks again Dr Gupta.
[…] This post was mentioned on Twitter by EP Lab Digest. EP Lab Digest said: RT @drjohnm: Highlights of the Boston 2011 AF symposium… It was a great meeting! http://ow.ly/3Gqdz #afib […]
Dr. Mandrola,
Great summary and coverage of Boston AF. Yes, Dr. Prystowsky is always entertaining, thought-provoking, and honest in that he shares what he thinks. Of course, I thought I was the only one that didn’t quite understand ALL of the basic science stuff. Great job. See you there next year.
Mellanie
Thanks for the informative summary of the meeting. With regards to your comments about Pappone results, what did he present and is there a paper reference to go with the presentation. Thanks.
I’m curious about the meaning of term “extensive ablation” used in your 1/19/11 blog. How might it differ from a conventional A-fib ablation? What are possible long-term implications (especially for us cyclists) with this type of approach?
P.S. I am coming to terms with a sense that my road riding, especially climbing, will never be the same after an PVIA/flutter ablation and a touch-up ablation w/ work in the LAA. Is in line with what your patients engaged in endurance sports have experienced?
Dr Pappone’s presentation discussed strategies on ablating long-standing atrial fibrillation. I don’t recall that he presented anything novel. He is known in the AF world for the remarkably positive success rates that he reports. Words that I have heard used to describe these results include striking, remarkable and even unbelievable; the same words that are used to describe winning seven Tours.
Campy…
In a 3-d reconstruction after extensive ablation, red-dots, (which depict an RF-lesion) obscure the entire left atrium. The advocates of this strategy purport better results, the nay-sayers (the minimalists) worry that these burns will diminish the squeezing function of the atrial muscle–which is one of the benefits of sinus rhythm. Since these approaches have not been compared head-to-head and adjudicated independently the best answer is not known.
Your observations about lower climbing prowess could be used by critics of extensive ablation to support their view about left atrial mechanical function. The hitch in this logic is that elite athletes are a not very generalizable group, as for them, even minute changes in cardiac function make huge differences in outcome. Sure, it’s conceivable that extensive ablation may reduce cardiac function enough to affect one’s ability to hold a wheel in a crit, but so would having AF–or a bad night sleep, or eating heavy cheese burrito the night before.
My experience with ablating elite athletes is too small to comment, but I can say without any doubt that competitive athletes do poorly with either a rhythm problem or anti-arrhythmic meds.
JMM
In your comment on ablating intermittent (paroxysmal) AF, the recurrence rate of AF was too high after initial ablation. Do you know if that applies to those who have a second or third ablation? Did they mention a percentage for success?
Steve,
Thanks. This is a good question. In general the recurrence rate after a second ablation procedure is much less than the index procedure. Here’s a stab at explaining why: Consider AF-ablation like building a fence–an electrical, not a mechanical one–around the pulmonary veins. When AF recurs it is usually because the fence developed a breach. The repeat ablation, therefore, has only to mend the breach, not build an entirely new fence. Picture spot-welding. So, assuming the rest of the fence holds up–and that is not a certainty–the likelihood of recurrence after the repeat procedure is less.
What I tell patients with paroxysmal AF is that the recurrence rate for the initial procedure is around 30%, and the recurrence rate after the second would be 5-10%. This all adds up to a 80-90% overall success rate.
High recurrence rates after AF ablation are much different than the exceedingly low rates after ablation of focal problems like SVT and Aflutter. These arrhythmias, unlike AF, do not require an encircling fence, just a single burn.
Hope this helps.
Wish the AF conference would rotate locations like HRS meetings. Who wants to fly to Boston in January?
I heard Pappone speak at ACC a couple years ago. IIRC, his 80-90% success rate required an average of 2.5 procedures per pt.
Interesting that no one commented on Multaq. Given the recent info re: liver failure, do you plan to start any new pts on it?
We did a drug utilization review at our facility. Found one pt on Multaq w/ LFTs 2x ULN. Sent the provider a message since the pt is not followed in cardiology. That may be the next step – restricting use to cardiology only.
As an electrophysiologist, patients seek me out to control their AF. This usually means using a “rhythm control” strategy, and in this regard, Multaq hasn’t proved helpful. This lack of efficacy quickly became evident, and the company started touting it for its safety profile compared to amiodarone. Now that strategy appears dubious.
Thanks for writing.